What Causes Fatigue and How Can I Treat It?

Modern life and the juggling of a career and family can be flat-out tiring. Now add an autoimmune disease like MS to the mix, and it’s no surprise you feel flat-out exhausted. You may be wondering what are the causes of fatigue and what can you do about it. Even though fatigue is an elusive symptom, there’s so much we can do to boost energy and get through our day better. So let’s talk about what causes fatigue and fatigue busters.
What does fatigue feel like?
It’s no secret that fatigue is one of the most common symptoms experienced by those of us living with MS. So naturally, it’s a topic that is top of mind, given it’s huge impact on quality of life.
Can you relate to any of these?
- You finish your day by sinking into your couch, asking “Why am I so exhausted?”
- Your fatigue is so all-consuming that it’s hard to get out of bed in the morning.
- It feels like a struggle just to take care of basic chores like caring for yourself and your family
You are not alone in feeling tired and drained. In fact, many of my patients tell me that among all of their symptoms, fatigue is the most debilitating of all. It can feel awful, if not demoralizing, when day after day passes and you feel completely depleted, unable to fulfill even the easiest tasks.
Fatigue is among the most complex of symptoms to study. And because so many different factors contribute to this symptom, it’s difficult to pinpoint its exact causes.
What’s more, people’s description of fatigue varies greatly, ranging from a lack of energy, to sleepiness, or even a sensation of weakness or heaviness in the body. Further complicating the matter, no laboratory tests exist to diagnose fatigue
Fatigue vs. Tired: What’s the difference?
So how do you know whether you’re tired or have bonafide fatigue? While the distinction is not always clear cut, here’s a general a breakdown:
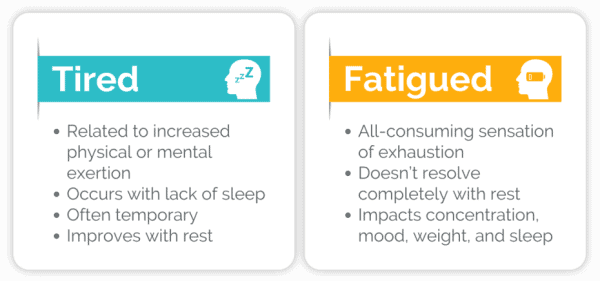
One way to determine whether you are fatigued or just plain tired is to pay attention to your symptoms.
- What words best describe what you are experiencing?
- What brings on your symptoms and what factors seem to help?
- What other symptoms beyond lack of energy are you experiencing?
Even if they seem unrelated, it’s helpful to track ALL your symptoms by taking notes in a diary or calendar.

If your symptoms persist, it’s important to see your doctor to rule out reversible causes of low energy and fatigue, such as an underactive thyroid, anemia, diabetes, etc. However if no reversible cause is found, your doctor may determine that you indeed are experiencing fatigue, which has real implications for self-care and quality of life.
Getting the right diagnosis is important
as this determines your treatment options.
While there are medications that can help, there are non-pharmaceutical approaches that can have equally potent if not more widespread benefits in the treatment of fatigue. More on this in a future blog.
Where does fatigue come from?
There is no single cause for fatigue. Rather, multiple environmental, cellular, and genetic factors interact to create the perfect storm that is fatigue.
There is no way of predicting who will experience fatigue, though having a chronic autoimmune disease like MS increases the risk. As mentioned earlier, there are no laboratory tests to shed light on this elusive condition.
Assuming reversible causes of fatigue have been ruled out by your doctor, we can then zoom in and look at some of the imbalances in body systems that contribute to fatigue.
Factors that Contribute to Fatigue
-
Mitochondria found inside your cells are tasked with producing energy for the body in the form of ATP molecules. Any insult or injury to these tiny energy factories can lead to an energy crisis, resulting in fatigue. Therefore the health and wellbeing of mitochondria is vital for a well-fueled body.
-
Both physical and emotional stress can tax the hormone system, which responds by altering levels of key hormones, such as cortisol. With prolonged stress, our adrenal glands, whose job is to produce cortisol, may fail to keep up. In integrative and functional medicine we call this “adrenal fatigue,” characterized by low levels of cortisol throughout the day that often correlate with fatigue.
-
The gastrointestinal (GI) system is intimately connected to every other system of the body. When the lining of the GI tract is damaged and becomes porous, a condition called “leaky gut” develops. As a result, the gut is no longer able to tightly regulate what can safely enter the body. This leads to overstimulation of the immune system and there can be loss of nutrients, both of which can lead to fatigue.
-
The gut microbiome plays a role in just about everything, including fatigue. These microorganisms living in our large intestine have coevolved with us and perform functions we cannot do on our own. Data shows that loss of certain beneficial microorganisms populating the large intestine correlates with fatigue. [1]
-
The immune system is also implicated in fatigue. In fact, inflammation created by the immune system may at least partially drive fatigue. In patients with chronic fatigue syndrome, inflammation in the brain is a key feature. [2]
-
Genetic mutations are also partly to blame. Certain gene mutations correlate with fatigue, although they are not proven to be true causes of fatigue. For example, mutations in the MTHFR gene are quite common in the general population. People who carry this mutation struggle with methylation, a process that is central to energy production. [3]
This is just a cursory list of some of the main players involved in fatigue, but is by no means an exhaustive. As you can see, it’s complex. In fact, it may even seem impossible to peel apart the layers and to get to the heart of what is causing fatigue.
Good news! An integrative approach SIMULTAENOUSLY addresses mulitple factors contributing to fatigue.

How do I figure out what caused my fatigue?
Take a look at this list above. Which one of these potential causes pertain to you?
Without undertaking a large battery of functional tests, (which I’m definitely NOT condoning), we CAN draw some conclusions based on your history and symptoms.
If you live with an autoimmune condition, it is likely that:
- Your mitochondria are not in tip-top shape. Think Dr. Wahl’s. Her book “Minding My Mitochondria” places the mitochondria front and center in the unfolding of MS. [4]
- Your gut microbiome is out of balance.
- Leaky gut is probably at play given that it’s one leg of the autoimmune triad. (hyperlink to autoimmune blog
- There are changes in hormones like cortisol and thyroid (even if not abnormal enough to warrant a diagnosis by your medical doctors)
- You struggle with methylation due to common gene mutations
- Your immune system is tipped towards creating inflammation because it has forgotten the rules around what to attack and what to leave alone.
Yes, this is a LOT to consider. But stick with me as I build the case below and in upcoming blogs for how we are going to tackle this thing called fatigue.
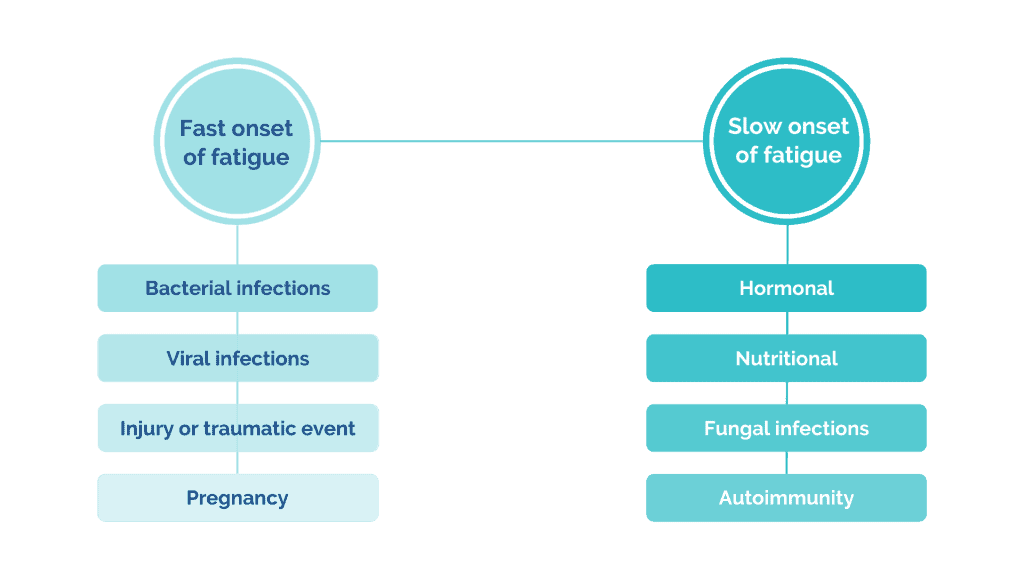
Sorting out YOUR causes of fatigue
Think back in time to when you first became aware of fatigue. Did it come on suddenly or did fatigue creep up on you over several months to years? The speed of onset can be an important clue as to what caused fatigue in the first place. On one end of the spectrum, the sudden onset of fatigue may be due to a bacterial or viral infection, injury or traumatic event, and even pregnancy. On the other end, a slower onset of fatigue may point towards hormonal, nutritional, fungal, and autoimmune issues as the culprits.
Keep in mind that the practice of medicine is rarely black and white, especially when it comes to something as complex as fatigue. What the most likely scenario is that there are multiple causes to your fatigue, spanning both ends of the spectrum.
Yup, I have fatigue. Now what?
If you’re feeling overwhelmed by all the different factors that go into fatigue, I don’t blame you – especially if your approach is to go after each imbalance separately.
But that’s NOT the approach we are going to take – because I know patients with fatigue who take as many as 30 different supplements, and I’m not sure they are any better off.
The TRUE Medicine approach uses lifestyle
to treat root causes at the cellular level.
What is this streamlined approach? It’s lifestyle.
 When you eat good food, prioritize restorative sleep, move your body every day, and manage stress, you simultaneously boost the health of your mitochondria, restore balance to the hormone system, improve gut health, promote the growth of friendly bacteria, and give the immune system a chance to turn off inflammation. There is no medication that can do what clean lifestyle habits can do for fatigue. Period.
When you eat good food, prioritize restorative sleep, move your body every day, and manage stress, you simultaneously boost the health of your mitochondria, restore balance to the hormone system, improve gut health, promote the growth of friendly bacteria, and give the immune system a chance to turn off inflammation. There is no medication that can do what clean lifestyle habits can do for fatigue. Period.
Think about your current state of health. No matter where you are on that continuum of poor to perfect health, there is always something you can do to move closer to better health.
How do we know thyat? Because your body is an incredible machine that is programmed to create health – IF you provide the right conditions. So tap into the wisdom of your body by trusting yourself and your built-in healing mechanisms to move you closer to better health.
Stay tuned for how nutrition, restorative sleep, and stress management all work to bring your body systems back towards balance to improve fatigue.
Sources:
- König RS, Albrich WC, Kahlert CR, et al. The Gut Microbiome in Myalgic Encephalomyelitis (ME)/Chronic Fatigue Syndrome (CFS) [published correction appears in Front Immunol. 2022 Mar 30;13:878196]. Front Immunol. 2022;12:628741. Published 2022 Jan 3. doi:10.3389/fimmu.2021.628741
- Lee CH, Giuliani F. The Role of Inflammation in Depression and Fatigue. Front Immunol. 2019;10:1696. Published 2019 Jul 19. doi:10.3389/fimmu.2019.01696
- Vangeel EB, Kempke S, Bakusic J, et al. Glucocorticoid receptor DNA methylation and childhood trauma in chronic fatigue syndrome patients. J Psychosom Res. 2018;104:55-60. doi:10.1016/j.jpsychores.2017.11.011
- Wahls, T. L. (2010). Minding my mitochondria: How I overcame secondary progressive multiple sclerosis (MS) and got out of my wheelchair. Tz Press.
- Toxins (Basel). 2019;11(3):147. Published 2019 Mar 5. doi:10.3390/toxins11030147
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
CTA statement
Nullam cursus massa sit amet risus vulputate, vitae convallis leo semper. Proin purus neque, varius at metus ac, maximus tempor nisl.



Responses